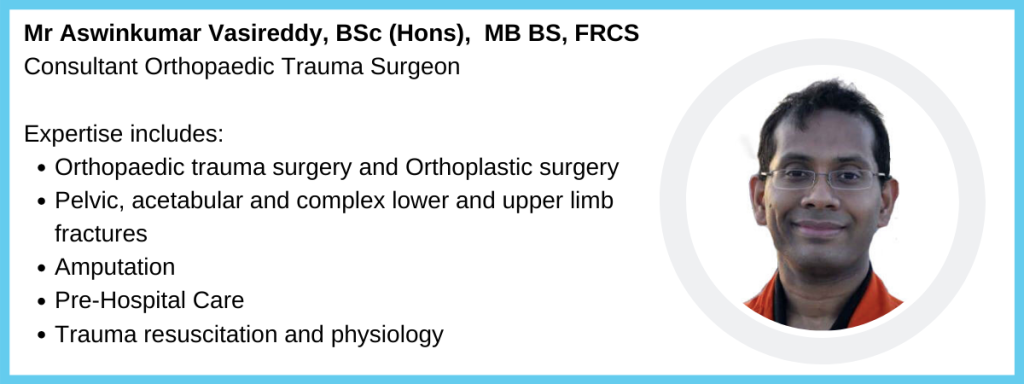
Compartment syndrome is a devastating limb threatening condition. It is infrequent and usually associated with fractures, predominantly of the tibia. It is a clinical diagnosis and if treatment is delayed or missed, it leads to significant long-term dysfunction. In this article, Mr Aswinkumar Vasireddy, Consultant Orthopaedic Trauma Surgeon, explains the condition and explores its medicolegal challenges.
Compartment syndrome occurs when excessive pressure builds up in an enclosed compartment within the body. The condition is an emergency usually requiring surgery to prevent permanent damage and, if left untreated, loss of body function. The condition usually develops quickly over the course of a few hours after injury. It is more common in men, in whom the annual incidence is 7.3 per 100,000, compared to 0.7 per 100,000 in women. Age is an important risk factor in the development of compartment syndrome, with patients below the age of 35 years being much more likely to develop the condition. The condition can also develop in children, although the presentation can be very different to that seen in adults.
Compartment syndrome is usually the result of swelling or bleeding following injury. It usually occurs as a result of an increase in the pressure within a given compartment. This increased pressure can be caused by bleeding, swelling or a tight cast , which acts to reduce the space within the compartment. Once this intracompartmental pressure reaches a threshold, it affects the blood flow in the limb leading to severe pain. If prolonged, the tissues are deprived of their blood supply and thus can be irreparably damaged.
Nearly 70% of cases are due to fractures, with the tibia being the most common site of injury. The mechanism of injury is equally distributed between high-energy and low-energy trauma. While it was once thought that open fractures carried a lesser risk of compartment syndrome, recent research has shown that this is not the case and that the intracompartment pressure is similar in open and closed fractures. It has also been shown that fracture reduction and manipulation can increase the risk of compartment syndrome.
The remainder of compartment syndrome cases usually arise following soft tissue injury, where arterial damage from high-energy trauma causes the development of a haematoma, which leads to increased pressure in affected compartments. In this type of injury, the compartment syndrome often develops in an unusual location, such as the thigh or foot. There is also a significant risk of compartment syndrome in intubated patients or those with a lower level of consciousness. As communication is difficult in these cases, doctors tend to keep a high level of awareness about the possibility of the condition developing. This is also true of paediatric patients, where the presentation of compartment syndrome differs from that in adults. Often, the only symptom is pain.
The early symptoms of compartment syndrome are non-specific, which can lead to a delay in diagnosis. Classic features of the condition, which include pain, pallor, paresthesias, paralysis and pulselessness (also known as the 5 ‘Ps’) all develop later in the course of the condition and are associated with irreversible damage. Although all these signs have a role in identifying the condition, the overall clinical picture is more important in making a diagnosis than the presence or absence of any one particular symptom. A diagnosis of compartment syndrome tends to be made over time, following the assessment of the evolving signs and symptoms, rather than in isolation at a single time point. Therefore, serial examinations, ideally performed by the same examiner, are crucial. The main focus of treatment for compartment syndrome is to relieve the pressure in the affected compartment. Constricting dressings, casts and splints must be removed from the affected area. Additionally, surgical intervention is usually required, in the form of a fasciotomy, in which long cuts are made in the fascia layer beneath the skin to release the excess pressure. UK national guidelines also exist to help provide guidance on diagnosis and treatment, including an emphasis on the importance of rapid treatment once the diagnosis has been made.
As well as the serious consequences of a missed diagnosis, an additional facet of compartment syndrome management nowadays involves minimising the risk of a negligence claim in these circumstances. While most orthopaedic surgeons will see cases of compartment syndrome during their career, medical negligence claims arising from the condition are relatively rare and account for around only 5% of all orthopaedic claims. However, these claims are much more likely to be settled in favour of the patient than other conditions, with about 50% resulting in a settlement. This compares to 25% of cases overall. Cases in which poor communication between doctor, nursing staff and patient has been identified are likely to result in a payment, as are those in which there is a failure to intervene after documentation of an abnormal physical finding. There is also a link between the time between onset of symptoms and performance of fasciotomy and the level of payment secured by the patient, with all cases in which fasciotomy was performed within eight hours being successfully defended. Therefore, early fasciotomy not only improves the outcome for the patient but also decreases the likelihood of a claim and the level of settlement.
About Medicolegal Partners
Mr Vasireddy specialises in the management of complex open/closed pelvic, acetabular, upper limb and lower limb fractures and amputations. He is also one of a small group of surgeons, and the only contemporary Orthopaedic Surgeon in the UK, who works as a HEMS (Air Ambulance) Pre-hospital Care Doctor.
To instruct him or any of our experts, please get in touch: info@medicolegal-partners.com
Further Reading:
Taylor, R. M., Sullivan, M. P., & Mehta, S. (2012). Acute compartment syndrome: obtaining diagnosis, providing treatment, and minimizing medicolegal risk. Current Reviews in Musculoskeletal Medicine, 5(3), 206–213. https://doi.org/10.1007/s12178-012-9126-y
Weingart, G., & Kumar, S. (2017). Acute Compartment Syndrome. Emergency Medicine, 49(3), 106–115.
