How a Pain Expert Can Assist in Fibromyalgia Cases

Fibromyalgia (FM) is a relatively common pain syndrome and affects around 3-5% of the population. It is much more frequent in women than men, and is more prevalent than other pain conditions such as rheumatoid arthritis. The main features of the disease are widespread pain and chronic fatigue. There is no known cause for FM and it is likely that multiple factors lead to the development of the condition in any one patient. Known risk factors include traumatic injury, surgery, illness, psychological trauma and anxiety, and sleep disturbance. There may also be a genetic element to the disease. The underlying mechanism of the disease appears to be sensitisation of the central nervous system, which remains in a state of high reactivity after an initial stimulus.
Although FM has been recognised for many years, diagnosis is often problematic and there is no definitive test for the condition available. However, for a patient, receiving a diagnosis of FM can be very helpful. It legitimises their condition and provides an explanation for the subjective symptoms they are experiencing. Once diagnosed, patients are often better able to cope with their condition, and are also able to access further treatments, some of which may only be available to those with a specific diagnosis.
However, many of the symptoms of FM are common to other conditions, such as chronic fatigue syndrome, rheumatoid arthritis and lupus. Thus, FM is often a diagnosis of exclusion and other conditions must first be ruled out. Furthermore, the presence and severity of pain cannot be measured objectively and a physician must rely on a patient’s subjectively reported experiences in order to arrive at a diagnosis. A pain expert is well-placed to distinguish between the similar characteristics of FM and other pain conditions, thus arriving at a correct diagnosis. In order to understand FM fully, a comprehensive evaluation of a patient’s pain, function and psychosocial context is required. Once other diagnoses have been discounted, FM is usually confirmed by the presence of pain in all four quadrants of the body lasting for at least three months.
Currently, no effective cure exists for FM and while various treatment options are available, none of these is entirely effective on its own. Instead, the main aims are to reduce symptoms and to lessen the impact that the condition has on the patient’s life. As FM has both physical and emotional aspects, it is now widely recognised that a multi-disciplinary approach to pain management has the highest chance of achieving a successful outcome for the patient. A pain consultant’s expertise will form a vital part of this. A doctor specialising in the complex area of pain has a unique understanding of how it can be managed using drugs, relaxation practices and physical therapies. It is also likely that a pain clinic will have a team of physical therapists, nurses and occupational therapists on their staff who will be able to treat all of the symptoms of FM. Although the expertise of a neurologist or rheumatologist may also be useful, neither field focusses specifically on FM, so it is possible that these practitioners may have little or no experience of the condition.
A common pharmacologic intervention for FM is treatment with tricyclic antidepressants. Although originally developed for use in depression, at a lower dose this class of drug has an effect on both pain and sleep disturbance, and may also reduce fatigue. However, tricyclics are also associated with a relatively high incidence of side effects. Newer antidepressants have fewer adverse effects but are less effective in providing pain relief. Anticonvulsant medications are also commonly used to treat FM, but their effectiveness is questionable. In addition, side effects can be a significant problem.
There is also some evidence that vitamin D supplementation may be helpful in treating FM. Vitamin D deficiency is extremely common, particularly during the winter months in northern latitudes. It is also strongly correlated with chronic pain in general. Although there is no good evidence that hypovitaminosis D causes FM, studies have shown that supplementation can lead to an improvement in some FM symptoms.
Non-pharmacologic interventions are equally important in the treatment of FM and are considered a necessity by some doctors. These might include stress management and physical exercise. There is some evidence in the medical literature that practices that aid relaxation, such as yoga, massage and acupuncture, may have a positive impact on sleep quality, fatigue and quality of life. Moderate physical exercise can also be very beneficial. One study showed that FM patients who performed tai chi, a mind-body practice that involves meditation and gentle movements, once or twice a week reported a greater improvement in pain than a group who undertook aerobic exercise sessions instead.
Although there is no definitive treatment for FM, a multi-faceted approach, which encompasses both pharmacological and physical therapies can be extremely beneficial to many patients. With appropriate treatment, those with mild to moderate pain are usually able to live a fairly normal life. It is clear that only a pain expert has the wide-ranging knowledge to ensure that diagnosis and effective management of this condition is achieved.
About Dr Jenner
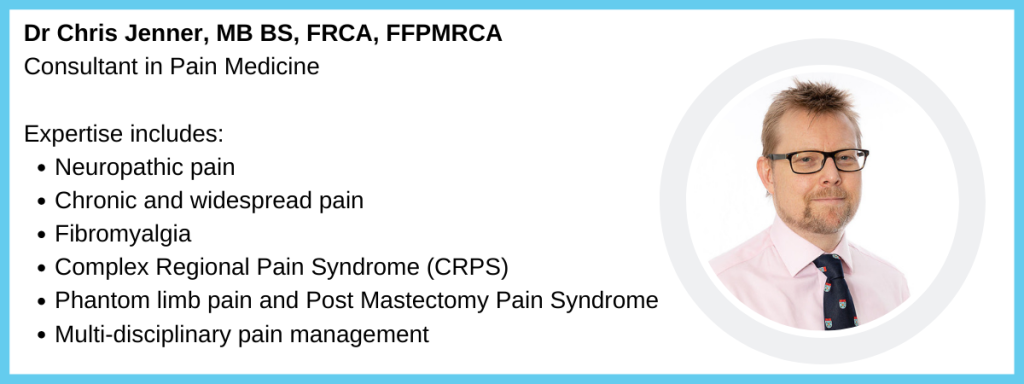
Read Dr Jenner’s full biography and download his CV.
Further reading
http://www.fmauk.org
Hauser, W., Sarzi-Puttini, P., & Fitzcharles, M.-A. (2019). Fibromyalgia syndrome: under-, over- and misdiagnosis. Clinical and Experimental Rheumatology, 37 Suppl 1(1), 90–97.
